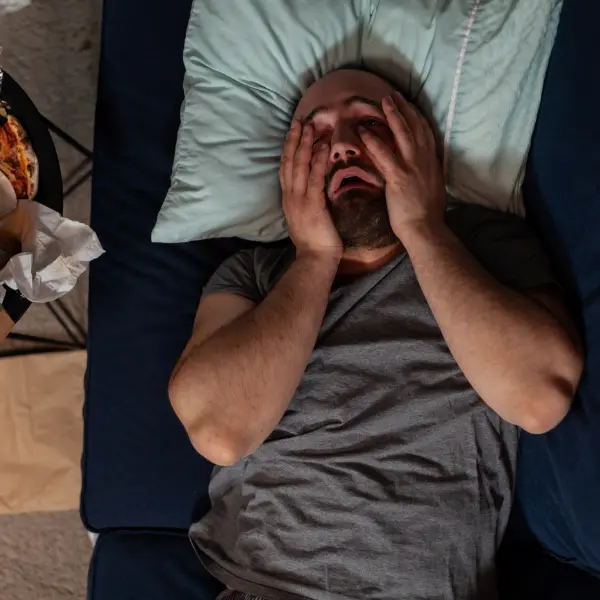
If you or your loved ones have faced drug addiction, you will surely understand how this messes up with your sleep cycles. The question is, when a drug addict is using, he/she should sleep better, right? So, how does this affect their sleep cycle by any chance? Developing healthy sleep habits can be challenging for those struggling with addiction, but it is a crucial step toward restoring natural sleep patterns and improving overall well-being.
Sleep Disturbances Caused by Substance Use Disorders
Substance use disorders often lead to sleep disturbances such as insomnia symptoms, excessive daytime sleepiness, and poor sleep quality during both active use and recovery.
Drug addiction disrupts natural sleep cycles by causing changes in neurotransmitters, hormones, and brain activity, leading to insomnia, reduced REM sleep, and other sleep disturbances.
Different types of drugs have varying effects, with stimulants like cocaine hindering sleep onset and decreasing REM sleep, while depressants like alcohol can disrupt sleep stages.
The Impact of Alcohol & Drug Abuse on Sleep Patterns
People who use alcohol tend to have more difficulty falling asleep and returning to restful slumber throughout the night than those who don't drink alcohol. Drug and alcohol abuse interferes with circadian rhythms, leaving the body less sensitive to daylight/dark cues, which trigger shifts in metabolism and secretion of melatonin (a natural sleep-inducing hormone).
Drinking increases the waking frequency, which in turn lowers the quality of sleep. Furthermore, alcohol can contribute to numerous health problems that contribute to poor rest. For instance, snoring and central sleep apnea are both conditions in which breathing stops occur while impairing cognitive function may result in impaired decision-making abilities, increasing the risk for relapse. Here are some alcohol withdrawal symptoms.
How Circadian Rhythms & Sleep-Wake Cycles Are Affected
Addictive substances alter circadian rhythms and disrupt sleep-wake cycles, resulting in irregular waking hours and poor regulation of the body’s internal clock.
Addiction to drugs such as alcohol and prescription and over-the-counter drugs can disrupt normal sleeping patterns. Users often report insomnia in addition to experiencing other physical and emotional challenges associated with substance abuse.
This may be because these substances interfere with circadian rhythms, which regulate natural sleep-wake cycles within the body.

Sleep Issues & Substance Withdrawal
Disruptions in slow-wave sleep, which is crucial for restorative deep sleep, are common in individuals recovering from substance abuse, further impairing their ability to achieve restful sleep.
Sleep problems in addiction recovery can be treated both behaviorally and medically at drug detox facilities. At these centers, professionals specialize in insomnia treatment while helping you break free of substance use patterns.
Schedule Appointment Now
1. Insomnia
Insomnia can be short or long-term and affects both men and women alike. It may result from lifestyle changes like travel or changing work schedules or from stress, depression, anxiety, or other mental health conditions.
Sleep and substance use are closely linked, as substance abuse can exacerbate sleep difficulties, including insomnia and sleep-disordered breathing, further impacting overall sleep quality and mental health. Addressing these intertwined issues is crucial for improving restful sleep and supporting recovery.
2. Sleep Apnea
Sleep Apnea occurs when your brain fails to send adequate signals to the muscles responsible for breathing. While less common than its obstructive counterpart, central Sleep Apnea still impacts many individuals.
- Especially older individuals and those who have had a stroke or take narcotic painkillers.
- It's particularly prevalent among the elderly.
- Sleep apnea and insomnia can both contribute to severe daytime fatigue and irritability, so if both apply.
- Your doctor will suggest conducting a comprehensive sleep evaluation.
Either alone or with the help of bed partners/roommates to provide accurate results that can help determine the most suitable treatment plan.
3. Restless Legs Syndrome
Restless legs syndrome (RLS) is an unpleasant, uncontrollable urge to move the legs or arms during sleep that causes discomfort. It can occur on either one or both legs and becomes worse at night.
- Although RLS affects people of any age, pregnant women and elderly adults are particularly prone.
- Although doctors still are unsure what causes RLS, genetics may play a part.
- About half of those with the condition have at least one immediate family member with RLS.
- Low levels of iron may also contribute; eating foods high in iron, such as meat, fish, beans, nuts, and iron-fortified breakfast cereals, can help.
RLS sufferers typically report finding temporary relief through stretching or moving their legs; however, it's essential to visit their physician for medical advice regarding this problem.

4. Narcolepsy
Daytime sleepiness caused by narcolepsy can severely hinder work and school performance and driving safety, so seeking professional advice to address withdrawal symptoms is important. Healthcare professionals may prescribe stimulant drugs like:
- Modafinil
- Armodafinil
- Dexamphetamine
- Methylphenidate
This is to keep you alert during the day. Sedatives such as low-sodium oxybate or sodium thiopental before driving long distances may also be recommended to alleviate them.
There are support groups and qualified counselors dedicated to narcolepsy in many areas. Moreover, work with your healthcare professional to devise a schedule for taking naps during the day, using medicine, and taking hypnotics or melatonin at night to reduce any disruptions in sleep patterns.
Why Establishing Healthy Sleep Habits is Crucial in Recovery
During sleep, the body repairs itself, and the brain processes emotions and memories, which is vital for emotional regulation and decision-making. Lack of quality sleep can lead to increased irritability, anxiety, and depression, all of which are common relapse triggers.
Moreover, sleep deprivation impairs cognitive functions, making it harder to resist cravings and maintain the motivation needed for recovery. Establishing healthy sleep habits can significantly enhance the recovery process. Consistent sleep patterns help stabilize mood and improve overall mental health.
Practices like maintaining a regular sleep schedule, creating a restful environment, and avoiding stimulants before bedtime can promote better sleep quality. Over time, these habits can lead to improved physical health, increased energy levels, and a stronger ability to cope with stress.
Treating Sleep Disorders in Individuals with Use Disorders
Effective treatment often involves a combination of behavioral therapies and, when necessary, pharmacological interventions. Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly recommended non-pharmacological approach that helps individuals identify and change thoughts and behaviors that interfere with sleep. This therapy has shown success in improving sleep quality without the risks associated with sleep medications.
Tips to Promote Sleep & Restore Restorative Sleep Cycles
Sleep is essential to mental well-being, particularly during the difficult process of recovery from substance abuse. Luckily, there are various things individuals can do to enhance their quality of sleep and promote a healthier mind during recovery.
Substance dependency disrupts sleep cycles and lowers the quality of non-rapid eye movement (NREM) rest, which may result in fatigue, depression, and anxiety.

Set a Regular Sleep Schedule
Set and stick to a regular bedtime and wake-up time each day, even on weekends, to train your body to fall asleep more naturally and feel revitalized upon awakening.
Establish a pre-sleep ritual, such as taking a warm bath or shower, drinking decaffeinated tea, practicing relaxation techniques, light reading and stretching exercises before bed, listening to relaxing music, and listening to relaxation audiobooks.
Lessen Your Screen Time
Avoid heavy screen use, movement, and snacking right before sleeping, as these may hinder restful slumber. In addition, try to limit or avoid caffeine and nicotine, as these stimulants may keep you up at night and keep you from falling asleep quickly.
Consult a Professional
Consulting an addiction specialist can assist individuals in understanding how drug abuse impacts sleep and creating healthier sleeping habits for long-term recovery. Furthermore, creating a relaxing environment and following a consistent sleep routine can significantly enhance the quality of rest.

Practice Exercises
Mindfulness and meditation techniques, as well as physical activities such as yoga and tai chi, may also help enhance sleep quality, strengthen immunity, and relieve stress, thereby decreasing the risk of relapse. Talk with your healthcare provider for the most appropriate solution when dealing with insomnia during recovery.
Avoid Caffeine
Under-restring can heighten cravings and alter decision-making processes, thus increasing the risk of relapse. Therefore, addiction treatment and aftercare must include activities to promote quality sleep habits, such as mindfulness meditation or keeping a gratitude journal before bedtime to relax and fall asleep easily. Furthermore, stimulants like caffeine may keep you awake all night and interrupt the sleep cycle.
Conclusion
You need quality sleep to recover fully. Addiction disrupts your natural sleep cycles, but you can take steps to restore them. Focus on building healthy sleep habits, follow a consistent routine, and address any sleep disorders alongside your addiction treatment. When you sleep better, you heal faster—mentally, physically, and emotionally.
Start Drug Addiction Recovery with Dragonfly Medical
If addiction is stealing your sleep, it’s time to take back control. At Dragonfly Medical offers comprehensive substance abuse treatment that addresses the whole person—mind, body, and sleep cycle included. Our team helps clients manage insomnia, restless legs, anxiety, and the many sleep disorders that can come with recovery.
We combine evidence-based medical care with holistic therapies to support deep healing—day and night. Call us today or reach out online to start your recovery journey. Because restful sleep isn’t just possible—it’s part of your path to long-term sobriety.



